What is PANS/PANDAS?
Written by Kate Shore - 30 April, 2024
If you’ve ended up on this page I’m guessing you might have recently noticed some sudden changes in your child — perhaps increased anxiety, obsessive-compulsive tendencies, or unexplained tics — and you’re feeling confused. These sudden shifts can be distressing and if you’re anything like many of the parents I see in my clinic, you’ve no doubt spent many hours trawling the internet in the middle of the night looking for answers. You may have come across the terms PANS syndrome or PANDAS disease, and wanting to know exactly what is PANS/PANDAS? You’re in the right place!
What is PANDAS and PANS all about?
PANS (Pediatric Acute-Onset Neuropsychiatric Syndrome) and PANDAS (Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections) are two interrelated conditions that affect the neuropsychiatric health of children. They are conditions of neuroinflammation and immune dysfunction, both characterised by the sudden onset of symptoms such as obsessive-compulsive behaviours (OCD), anxiety, mood swings, and motor or vocal tics. They often strike children between the ages of 3 and 14, catching families off guard with its unexpected onset.
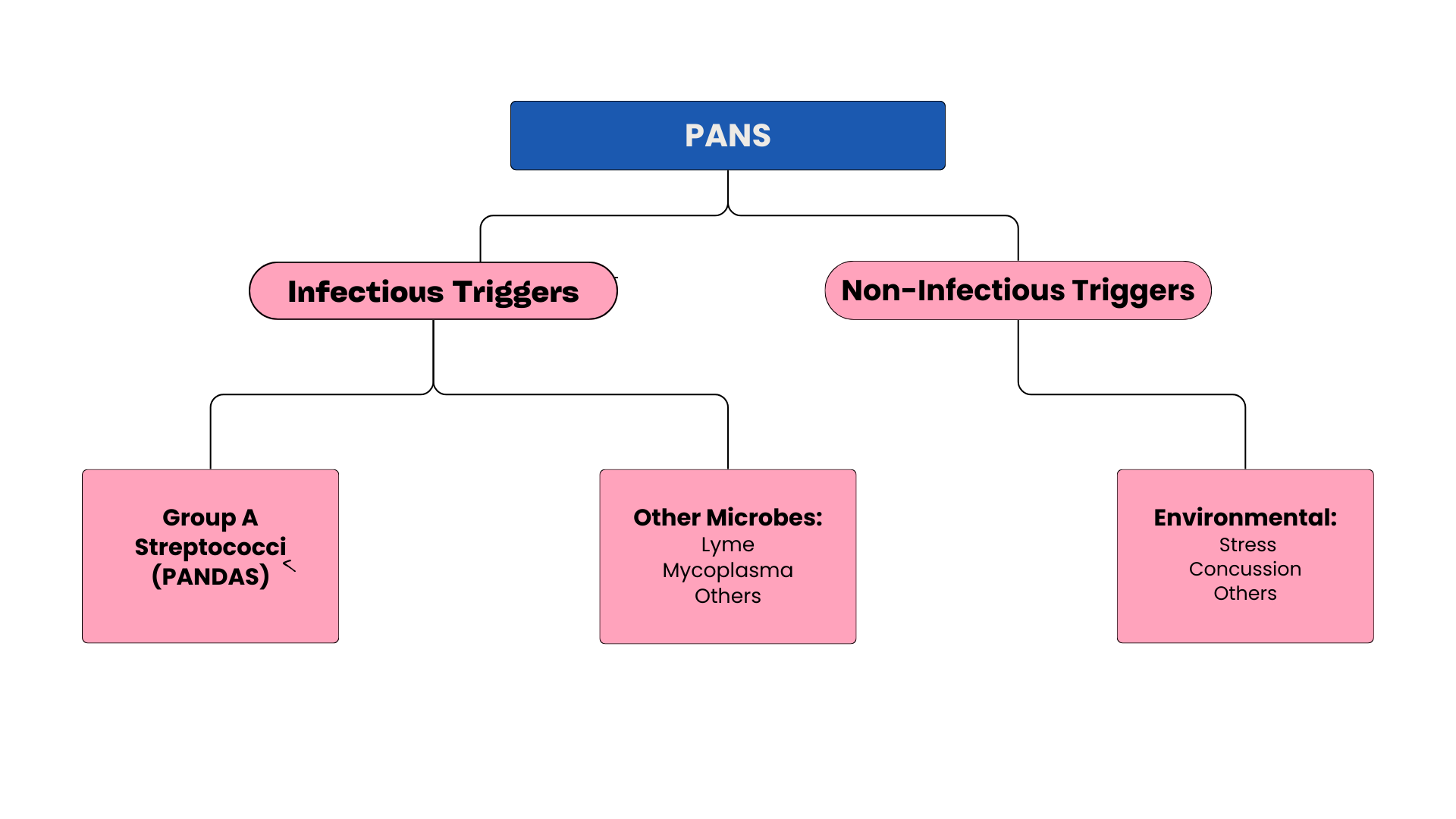
PANS and PANDAS are two distinct conditions that are often used interchangeably but actually vary slightly in their definition and classification. PANS is the overarching umbrella term for this neuropsychiatric presentation, and PANDAS is a subset of PANS where the onset occurs specifically following streptococcal infection.
What is common to these conditions is that symptoms typically occur quickly following an immune or inflammatory challenge, such as a sore throat, school sores or other viral infections. Certain infections, like strep throat, as well as other environmental exposures, trigger an immune response in susceptible children, leading to the sudden onset or exacerbation of neuropsychiatric symptoms.
What does PANS stand for?
PANS stands for Pediatric Acute-Onset Neuropsychiatric Syndrome, which can be broken down to more easily understand its significance:
The term "Pediatric" highlights the fact that PANS primarily affects children, typically between the ages of 3 and 14. It's important to recognise that children are particularly vulnerable to this condition, highlighting the importance of early detection and intervention.
"Acute-onset" emphasises the rapid and unexpected nature of the onset of symptoms. One day, your child may be perfectly healthy, and the next, they're experiencing intrusive thoughts, compulsions, and anxiety. This abrupt shift is disorienting for both children and their families.
"Neuropsychiatric” refers to the array of symptoms that children with PANS experience, ranging from OCD and anxiety to mood disturbances and cognitive deficits. Typically these symptoms are predominantly neurologically, or beginning in the mind.
And “syndrome'“ indicates that this distinct group of symptoms consistently occur together.
How common is PANS/PANDAS?
Exactly how common PANS is, is not completely clear, however, estimates suggest PANS affects approximately 1 in 200 children (1)
Determining the precise prevalence of PANS and PANDAS presents a significant challenge due to the complexity of the diagnostic process and lack of experience and awareness of PANS within the medical community. PANS is often overlooked or misdiagnosed by medical professionals due to the assumption that psychiatric symptoms lack an underlying medical cause. This misconception can lead to underreporting and underrecognition of these conditions, resulting in inaccurate prevalence estimates.
To get an understanding of possible prevalence we can look to research and longitudinal studies on children with OCD. Affecting approximately 2% to 4% of children under the age of 10, it has been speculated that 25% of cases of OCD in children may be related to Group A Streptococcus, suggesting PANDAS can be as common as 5 to 10 per 1000 children (2). In another study of 3200 children, 12 children were identified with acute neuropsychiatric or behavioural symptoms suggestive of PANDAS over a three-year period. This research estimated the incidence of PANDAS to be 4 per 3,200 children or approximately 1 in 1000 (3).
These estimates however are based on research where the onset of symptoms is associated with confirmation of streptococcus infection. Strep throat is typically confirmed through a throat swab test, which may not always be performed in every case of sore throat. Additionally, some children may have strep throat but never seek medical attention or undergo testing, leading to underreporting of cases.
Additionally, this data set only refers to research looking at PANDAS; it does not take into account the onset of symptoms following other immune triggers and hence does not capture the full picture of PANS in children. To understand the true impact and prevalence, more comprehensive research is needed, but it is much more likely that estimates of 1 in 200 are more accurate.
When was PANDAS discovered?
The history of PANS/PANDAS traces back to the 1990s when the initial description of PANDAS emerged from over a decade of research by Dr Susan Swedo and her colleagues at the National Institute of Mental Health (NIMH) (4). This pivotal discovery established a connection between children experiencing sudden behavioural changes and rapid-onset OCD, often accompanied by tics and psychological disturbances following infections with Group A streptococcal (GAS) infections. The onset of OCD symptoms following a GAS infection was of particular interest due to similar findings in research on Sydenham chorea (SC), a rare neurological disorder characterised by its sudden onset in childhood. Swedo’s research was able to draw from longitudinal studies of OCD and investigations of SC which helped give credibility to her findings (9). These insights led to the formulation of diagnostic criteria for the PANDAS subgroup, highlighting the abrupt onset and relapsing-remitting course of neuropsychiatric symptoms following infectious triggers (5).
While attention initially focused on strep infections, further explorations broadened the scope to include other infectious and non-infectious triggers. Reports of OCD and tic disorders associated with mycoplasma infections or chronic Lyme disease surfaced, and the term Pediatric Acute-onset Neuropsychiatric Syndrome (PANS) emerged to include a broader spectrum of acute-onset neuropsychiatric disorders (6).
The growing awareness and professional consensus led to the inaugural National PANS conference hosted by Stanford University in 2013. This landmark event saw collaborative efforts from leading PANS experts to establish clear diagnostic guidelines and improve support for affected families (7). Today, PANS includes specific diagnostic criteria, helping medical providers in navigating the complexities of pediatric neuropsychiatric disorders (8).
How long does PANS last?
The duration of PANS/PANDAS can vary widely among children, ranging from weeks to months or years. Some children may experience a single episode of acute-onset symptoms followed by a period of remission, while others may face recurrent episodes or persistent challenges requiring ongoing management and support.
Early detection, comprehensive assessment, individualised treatment plans and adherence to treatment protocols are critical to improving outcomes and promoting the long-term well-being of children affected by PANS/PANDAS syndrome, and eventually remission.
Patient and Family Support
There is no doubt that the impact of PANS/PANDAS extends beyond the individual child to affect their entire family, highlighting the importance of good support networks and collaborative intervention to improve quality of life, not only for children with PANS but their whole family. Some suggestions to help navigate this overwhelming time include:
Seek out healthcare providers who are knowledgeable about PANS/PANDAS disease and can offer support, guidance, and evidence-based interventions.
Connect with other families through support groups, online communities, and advocacy organisations to share experiences, resources, and coping strategies.
Prioritise self-care for yourself and other family members, recognising the emotional toll of navigating these complex conditions.
Research Advances
Despite the complexities of PANS/PANDAS disease, there is reason for hope on the horizon:
Ongoing research continues to explore the mechanisms underlying PANS/PANDAS and develop treatment approaches and therapeutic interventions. Researchers are continuously exploring novel biomarkers, neuroimaging techniques, and immune-modulating therapies to target the underlying pathophysiology of these conditions.
Clinical trials are underway to evaluate the safety and efficacy of emerging treatments, including immunomodulatory agents, anti-inflammatory interventions, and behavioural therapies, offering new hope for children and families affected by PANS/PANDAS.
By staying informed about the latest research findings, clinical trials, and treatment developments through reputable sources, academic institutions, and advocacy organisations, you can empower yourself with knowledge.
This article is part of a series on all things PANS and PANDAS. Part 2, "PANS/PANDAS Symptoms & Signs: A Checklist For Parents’ is all about the unique patterns and symptoms of PANS. You can continue reading the series by clicking through here.
This series is for educational purposes and does not constitute individual health advice. PANS and PANDAS are complex conditions, and it is important to seek the advice of a practitioner to assess what is right for your child. If you have questions, speak with your primary healthcare practitioner or book a free chat here where we can discuss the individual circumstances of your family.
More about Kate Shore - Paediatric Naturopath:
Kate Shore is a children’s naturopath with a special interest and clinical focus on working with kids to improve their mental health. Kate received her Bachelor of Health Science from Torrens University and has established her practice in North Warrandyte, Melbourne, where she sees clients both locally and all over the world. Her approach draws heavily on nutrigenomics, microbiome testing, nutritional foundations, and lifestyle support. She works with a range of children and conditions, from PANS/PANDAS, OCD, tics, anxiety and depression, ADHD and autism.
If you want to get in touch or have any more questions about the above, you are welcome to get in touch here or make an time for a free chat here.
If you want to keep learning, keep reading the research here:
These references and resources provide a comprehensive overview of PANS/PANDAS, offering valuable insights, evidence-based interventions, and avenues for further exploration and support. By tapping into these sources, you can empower yourself with knowledge, advocate for your child's needs, and navigate the complexities of PANS/PANDAS with confidence and resilience.
PANDAS Network. (n.d.). Retrieved from https://www.pandasnetwork.org/
Westly, E. (2009). From throat to mind: Strep today, anxiety later. Sci. Am. Retrieved from https://www.scientificamerican.com/article/from-throat-to-mind/
Wald, E. R., Eickhoff, J., Flood, G. E., Heinz, M. V., Liu, D., Agrawal, A., Morse, R. P., Raney, V. M., Veerapandiyan, A., & Madan, J. C. (2023). Estimate of the incidence of PANDAS and PANS in 3 primary care populations. Frontiers in pediatrics, 11, 1170379. https://doi.org/10.3389/fped.2023.1170379
Swedo, S. E., Leonard, H. L., Garvey, M., Mittleman, B., Allen, A. J., Perlmutter, S., Lougee, L., Dow, S., Zamkoff, J., & Dubbert, B. K. (1998). Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections: clinical description of the first 50 cases. The American journal of psychiatry, 155(2), 264–271. https://doi.org/10.1176/ajp.155.2.264
Swedo, S. E., Seidlitz, J., Kovacevic, M., Latimer, M. E., Hommer, R., Lougee, L., & Grant, P. (2015). Clinical presentation of pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections in research and community settings. Journal of child and adolescent psychopharmacology, 25(1), 26–30. https://doi.org/10.1089/cap.2014.0073
Swedo, S. E., Leckman, J. F., & Rose, N. R. (2012). From research subgroup to clinical syndrome: modifying the PANDAS criteria to describe PANS (pediatric acute-onset neuropsychiatric syndrome). Pediatr Therapeut, 2(2), 113. http://dx.doi.org/10.4172/2161-0665.1000113
Chang, K., Frankovich, J., Cooperstock, M., Cunningham, M. W., Latimer, M. E., Murphy, T. K., Pasternack, M., Thienemann, M., Williams, K., Walter, J., Swedo, S. E., & PANS Collaborative Consortium (2015). Clinical evaluation of youth with pediatric acute-onset neuropsychiatric syndrome (PANS): recommendations from the 2013 PANS Consensus Conference. Journal of child and adolescent psychopharmacology, 25(1), 3–13. https://doi.org/10.1089/cap.2014.0084
Swedo, S. E., Frankovich, J., & Murphy, T. K. (2017). Overview of Treatment of Pediatric Acute-Onset Neuropsychiatric Syndrome. Journal of child and adolescent psychopharmacology, 27(7), 562–565. https://doi.org/10.1089/cap.2017.0042
Swedo, S. E., et al. (2012). Identification of children with pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections by a marker associated with rheumatic fever. American Journal of Psychiatry, 169(2), 269-276. https://pubmed.ncbi.nlm.nih.gov/8988969/