How To Treat Concussion in Kids - Signs, Treatment Protocol & Support for Delayed Symptoms & Post Concussion Syndrome
Written by Kate Shore - 17th July, 2025
ARTICLE INDEX: What is a Concussion? | Signs & Symptoms | When to Seek Help | Do I Need to Keep My Child Awake? | Diagnosis | Concussion Protocol | Return to School | Return to Sport | Long Term Side Effects | Post-Concussion Syndrome | Supporting Recovery at Home | The Best Foods for Concussion Recovery | Natural Supplements for Concussion
If you've landed here, chances are your child has taken a bump to the head and you're wondering what to do next. Concussions can be scary for both parents and kids. Even when you're told it's “just a mild concussion,” things might not feel so mild when your child isn’t quite bouncing back, and struggling with longer term symptoms weeks or months later. We often hear parents say, “They said it wasn’t serious, but something’s not right.”
Whether it was a fall from a bike, a bump on the sports field, or a rough tumble at home, knowing what a concussion is and how to care for your child’s brain after a head injury is key. Concussion recovery isn’t always straightforward, but there is a lot you can do to support healing. Understanding what’s happening inside the brain, how concussions can impact mood, sleep, and even gut function, and which foods and natural supplements can nourish brain health can make a difference in how your child recovers.
What is a Concussion?
A concussion is a type of mild traumatic brain injury that occurs when the brain moves rapidly within the skull, typically due to a bump, blow, or jolt to the head or body. This sudden movement can cause chemical changes in the brain, damage to brain cells, and a temporary disruption in brain function.
Importantly, concussions don’t always involve loss of consciousness. In fact, most children with concussions are awake and aware, but may seem a bit “off” - they might only complain of a headache, feel dazed, or have trouble concentrating.
When it comes to concussion, kids aren’t just small adults, and there are a few important reasons why their injuries need extra attention. Their brains are still developing, making them more vulnerable to injury and often slower to recover. Structural differences, such as softer skulls, immature brain tissue, and weaker neck muscles, can affect how force is absorbed and how symptoms present (1). In fact, studies suggest it takes significantly more force to produce symptoms in children, meaning that when symptoms do appear, the impact may have been more substantial (2). This highlights the need for age-appropriate, cautious care to support full recovery and reduce the risk of long-term effects (3).
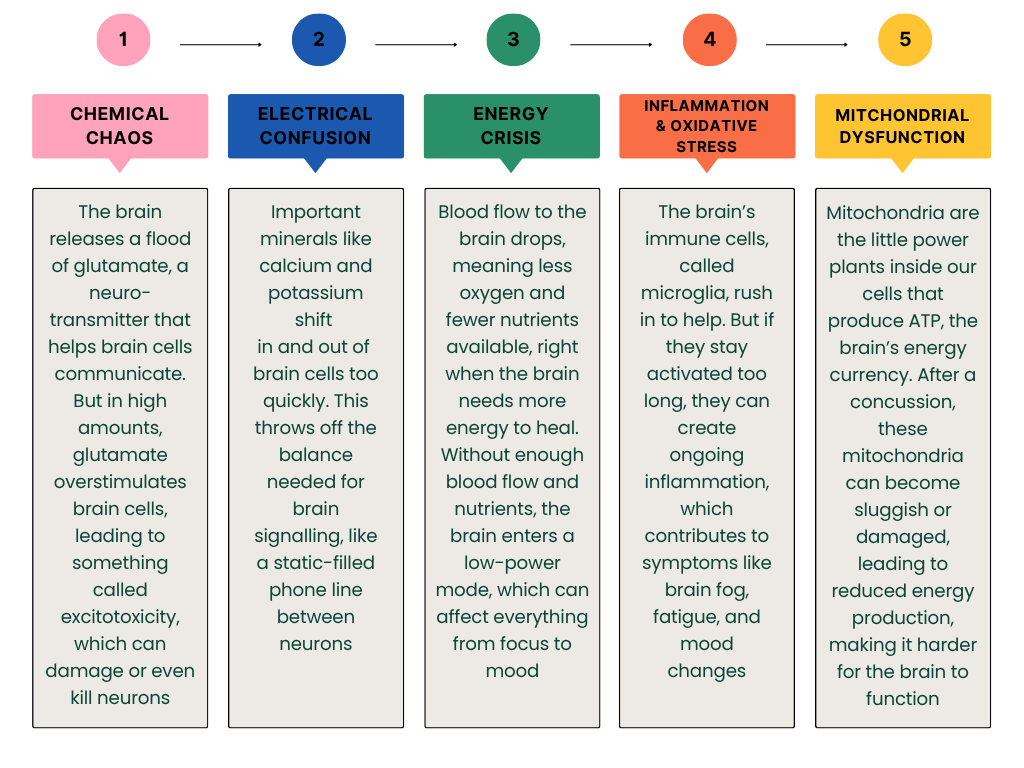
What Actually Happens in a Concussion?
(Warning: we’re about to get a little nerdy - because understanding the “why” behind the symptoms really matters.)
When a child experiences a concussion, it’s more than just a knock to the head. Inside that little skull, the brain - a soft, delicate organ - gets shaken; a bit like jelly wobbling inside a jar. This sudden movement kickstarts a chain reaction of chemical and physical changes that disrupt how the brain normally works.
Here’s what’s happening under the surface:
While this all sounds complex (and it is!), understanding these mechanisms is key to a more targeted and effective recovery. It helps us identify which areas or systems may need extra support and move beyond a general, one-size-fits-all approach. This allows care to be tailored to individual needs, especially when symptoms linger or fluctuate. It also helps explain why, for some children, rest alone isn't always enough for full and lasting recovery.
How Can Kids Get a Concussion?
Interestingly, concussions don’t always come from the dramatic, slow-motion sports moments we see on TV. They can happen in all sorts of everyday ways - some obvious, some totally unexpected (and yes, some involving siblings and flying toys).
Here are some of the common causes, and some more unexpected ones too:
Falls – off bikes, bunk beds, couches, skateboards, trampolines, or that one wobbly chair they absolutely had to climb.
Sports injuries – particularly common in contact sports like football, soccer, rugby, basketball, netball, and gymnastics.
Motor vehicle accidents – even low-speed bumps can jolt a child’s head enough to cause a concussion.
Being hit by an object – such as a ball, a door, or even a surprise airborne LEGO projectile.
And here’s something that often surprises parents: a child doesn’t have to hit their head directly to sustain a concussion. A sudden jolt to the body, like whiplash from a fall or being tackled hard in a game, can cause the brain to move rapidly inside the skull. It’s that shaking motion, not just the impact, that leads to the injury.
In short, if there’s been a big bump, a hard hit, or a fast fall, and your child seems “off” afterwards, it’s worth considering a concussion, even if they didn’t lose consciousness or seem hurt at the time.
Signs and Symptoms of Concussion
Every child experiences a concussion a little differently, which can make it tricky to spot, especially if symptoms aren’t obvious right away. Some kids bounce up after a fall and seem fine at first, only to develop signs like a headache, mood changes, or confusion later that evening or even days afterwards. These delayed concussion symptoms can be subtle, which is why close monitoring over the first 48–72 hours is so important.
Some of the most common signs to look out for are:
Headache - the number one complaint after a concussion.
Dizziness or balance problems – they might seem unsteady or complain that the room is spinning.
Nausea or vomiting – not always present, but can show up in the early stages.
Sensitivity to light or noise – bright lights or loud sounds may suddenly feel overwhelming.
Irritability or mood changes – emotional ups and downs, crying more easily, or feeling unusually frustrated.
Sleep issues – either sleeping more than usual or struggling to fall or stay asleep.
Brain fog or confusion – slower thinking, trouble concentrating, or feeling “out of it.”
Memory difficulties – forgetting things they’d normally remember or trouble recalling what happened during the injury.
If your child seems not quite themselves, even if the bump seemed minor, it’s always worth getting them checked.
What Should I Do If My Child Has a Concussion?
If you think your child may have a concussion, there’s no need to panic, but it is important to take it seriously and respond appropriately. Most concussion in children are mild and resolve well with the right support in the early stages, but prompt attention can make a big difference. Early injury assessment is associated with improved concussion recovery time(4).
Here are the first things to focus on:
Stop the activity immediately - If your child is playing sports or being physically active, have them sit out right away to prevent further injury.
Keep them quiet and calm - Find a quiet, safe space and help your child rest. Avoid stimulation like loud music, screens, or bright lights in the early hours.
Monitor symptoms closely - Stay with your child for the first few hours. Watch for changes in mood, behaviour, speech, balance, or awareness.
When to Seek Medical Help
While most concussions are considered low-grade or uncomplicated, it’s important to recognise when symptoms might point to something more serious, and require further assessment and medical care. Always seek help immediately if your child:
Loses consciousness
Vomits more than once
Seems very drowsy or difficult to wake
Is confused, disoriented, or behaving unusually
Has trouble walking, speaking, or using their limbs
Develops a severe or worsening headache
Has a seizure
Experiences loss of vision or double vision
Trust your instincts - if your child seems "off," it's always better to err on the side of caution. If symptoms are mild but lingering, such as persistent headache, dizziness, mood changes, or fatigue, it’s still important to check in with a health professional experienced in kids concussion. Early assessment helps confirm the diagnosis, guide recovery, and rule out more serious complications.
Should I Keep My Child Awake After a Concussion?
This is one of the most common and persistent myths about concussion care. But the short answer is: No, you don’t need to keep your child awake all night after a concussion (5).
In the past, parents were told to prevent sleep in case a child “slipped into a coma.” But we now know that sleep is actually one of the most powerful tools for brain healing. During deep sleep, the brain clears out metabolic waste, reduces inflammation, and begins repairing damaged tissue. In fact, restricting sleep can delay recovery and worsen symptoms like headaches, irritability, and fatigue (6).
If your child has been evaluated by a doctor and shows no signs of serious brain injury, it’s safe - and encouraged - to let them sleep, but check on them every few hours to ensure they’re rousable (they stir or respond when you gently wake them). If they’re difficult to wake or seem unusually drowsy, call your doctor or seek emergency care.
How Are Concussions Diagnosed?
One of the trickier things about concussions is that there’s no single, clear-cut test for diagnosis. Unlike a broken bone that shows up on an X-ray, concussions don’t usually appear on scans because they affect how the brain works, not how it looks.
Diagnosis is based on a combination of your child’s symptoms, what happened during the injury, and a thorough clinical assessment. In practice, healthcare providers often use tools like the SCAT5 or Child SCAT5 (for kids under 13) to guide their evaluation. These tools help assess:
Memory and concentration – Can your child remember words or events? Are they able to focus?
Balance and coordination – Are they a bit wobbly or unsteady?
Neurological signs – Are pupils reacting normally? Any unusual eye movements or speech changes?
Mood and behaviour – Have they become more emotional, withdrawn, or irritable?
In more serious cases, or if there’s concern about a skull fracture or bleeding, a CT or MRI scan might be ordered. But in most situations, imaging isn’t necessary and often doesn’t show anything anyway, as it doesn’t detect the functional changes caused by a concussion.
How to Treat a Concussion in a Child
The initial treatment for a concussion focuses on rest, monitoring, and a gradual return to normal activities. The first few days really matter, and a bit of rest, some gentle downtime, and keeping an eye on how they’re feeling is the priority. Every kid bounces back a little differently, but recovery generally follows these key steps:
The First 48 Hours: Rest (But Not Too Much!)
Concussion recovery starts with rest and careful monitoring, but the old advice of total isolation in a dark room has changed. While it’s important to take it easy for the first 24–48 hours by reducing physical activity, limiting screens, and avoiding anything too mentally demanding, too much rest can actually slow healing (7).
Instead of complete bed rest, support your child with a calm environment and encourage low-stimulation activities that don’t worsen symptoms.
Easing Back In: Light Activity
Once they’ve had a day or two to rest, gentle activities like listening to music, drawing, chatting with a friend, or going for a short walk can help ease them back into normal life.
Let symptoms guide the pace. If anything makes them feel worse, scale back and try again later. The goal is gradual reintroduction, not rushing, but not hiding away either.
Beyond the First Few Days: Monitoring Progress
Recovery times can vary, but most children start to feel better within a few days to a week. During this time, it’s important to:
Watch for any worsening symptoms, especially changes in behaviour, mood, balance, or headaches.
Follow a return to learn and return to play protocol if your child is in school or sports.
If symptoms persist beyond 2–3 weeks or interfere with daily life, it’s time to check in with a concussion specialist or pediatrician.
If you’re looking for an easy way to track symptoms, monitor progress, and know when to seek help, check out the HeadCheck app. Developed by the Murdoch Children’s Research Institute and backed by the AFL, it’s designed specifically for parents to help recognise the signs of concussion and support safe recovery at home. You can log symptoms daily, get reminders, and access step-by-step guidance for return to school or sport, all in one place. It’s free and easy to use, and a great tool for peace of mind while your child heals.
You can learn more or download at headcheck.com.au.
Concussion Protocol for Kids
Once the first period of rest has passed, it’s common to feel unsure about what comes next. A structured concussion protocol can provide clarity and confidence, offering clear steps to guide your child’s recovery and help you know when it’s safe to return to schoolwork, screens, or sports.
Without a plan, it’s easy to unintentionally do too much, too soon, especially if symptoms seem mild. But pushing through before the brain has fully recovered can prolong healing, worsen symptoms, and increase the risk of longer-term issues. This is especially important for children, whose developing brains are more sensitive to inflammation, metabolic stress, and repeat injuries.
Leading experts such as the Royal Children’s Hospital, Royal Australasian College of Physicians, and Australian Institute of Sport strongly advise a step-wise, symptom-guided return to daily activities. These guidelines are built on extensive research showing that both mental and physical rest, followed by gradual, monitored reintegration, lead to better outcomes in kids and adolescents (8).
Return to School Guidelines
When your child is ready, it’s time to start easing back into their usual routine, beginning with school. Returning to the classroom after a concussion can be just as tricky as returning to sports, so it’s best to take it slow and be guided by their symptoms.
This means starting with shorter school days or reduced workloads, taking regular breaks, and temporarily limiting screen use or noisy environments if they trigger symptoms. As recovery progresses, cognitive demands can be gradually increased.
Each child’s timeline will be different, so flexibility is essential, and regular communication with teachers or school staff can make the transition smoother.
Return to Sport Guidelines
One of the most common (and stressful) questions is: “When can my child go back to playing sport?”. And to put it simply, the answer is not until their brain is fully healed. And unfortunately, “feeling better” doesn’t always mean fully recovered.
Whether it’s footy, gymnastics, or a weekend skatepark session, returning to sport too early is one of the biggest risk factors for re-injury, and potentially more serious long-term effects. That’s why current Australian guidelines recommend a minimum of 21 days before returning to contact or collision sports after a concussion. This conservative approach reflects growing evidence that children and adolescents are more vulnerable to prolonged recovery and complications from repeated head trauma (9), even if they seem “fine” on the surface.
After a concussion, kids should follow a gradual concussion return to play protocol that prioritises brain healing and safety. The Australian Concussion Guidelines for Youth and Community Sport outline a staged return-to-play protocol, which includes:
Complete symptom resolution at rest.
Medical clearance from a qualified healthcare professional.
Graduated return to activity, starting with light aerobic exercise and progressing through sport-specific drills, non-contact training, and finally, full-contact practice.
Each stage should take at least 24 hours, and any return of symptoms should prompt a step back to the previous stage.
*According to the Australian Concussion Guidelines by AIS, children and teens under 19 shouldn’t return to stage 5 and full contact training until they’ve been completely symptom-free at rest for at least 14 days - that is not 14 days from the time of concussion, but 14 days from when there are no symptoms at all.
Why Clearance Matters
We know it can be tough when kids are eager to get back to school and sports, but medical clearance isn’t just a box to tick. Even though it can feel like an unnecessary wait, it’s an important part of making sure your child’s brain has healed properly. Even if your child feels “back to normal,” hidden issues like slower reaction times or lingering cognitive fatigue can still be present.
Medical clearance ensures all concussion symptoms have completely resolved, and brain function has returned to pre-injury levels. This can help prevent serious risks and prolonged recovery that can affect long-term well-being.
Concussion After Effects in Kids
Fortunately, most children recover from a concussion within a couple of weeks. They get some rest, take it easy, and soon enough they’re back on their bike, back on the field, or back to their usual whirlwind selves.
But for some, recovery isn’t so straightforward, and some children can continue to experience long term effects of concussion weeks, or even months, after the initial injury in areas like emotional regulation and gut-brain dysfunction.
Why Is My Child So Sensitive, Moody, or Anxious After a Concussion?
Concussions aren’t just physical injuries; they can also disrupt the brain’s emotional balance. While changes in memory or focus are expected, parents are often caught off guard by shifts in mood. Research shows that around 30–50% of children experience emotional changes such as anxiety, irritability, low mood, or trouble regulating their emotions after a concussion (10), even if their thinking and memory seem fine. This is because the areas of the brain that help with emotional control, stress regulation, and sleep, such as the prefrontal cortex, limbic system, and hypothalamus, can all be affected by head trauma.
The nervous system can also become dysregulated, particularly the part that controls the body’s stress response (fight, flight, or freeze). When this system is out of balance, it can lead to symptoms like noise sensitivity, difficulty settling, increased irritability, or even panic-like episodes.
Children may not be able to explain what’s happening, but you might notice:
Emotional outbursts
Fear of going to school or loud environments
Increased clinginess
Difficulty sleeping or relaxing
Sudden anxiety or sadness
That’s why it’s just as important to support your child’s nervous system and emotional well-being as it is to treat physical symptoms like headaches or fatigue.
How Concussion Affects the Gut–Brain Axis
Another unexpected symptom of concussion after effects is gastrointestinal signs. When your child bangs their head, the gut might seem like the last thing you'd think to worry about. But here’s the thing: the brain and gut are in constant conversation through the gut-brain axis, a complicated network involving nerves, hormones, and immune cells. Kinda like two kids with walkie-talkies, only the signal gets fuzzier when things go wrong. When inflammation or injury occurs in one, it can ripple through to affect the other.
After a concussion, studies have shown that head trauma can:
Increase intestinal permeability (aka “leaky gut”) - Traumatic brain injury, even mild, can disrupt the integrity of the gut lining (11), which then allows inflammatory substances and toxins to enter the bloodstream more easily.
Disrupt microbiome balance - Concussions can disrupt the balance of beneficial bacteria (12), allowing pro-inflammatory species to take over, contributing to increased inflammation.
Alter gut motility and trigger digestive symptoms - Some children experience changes in how quickly or slowly food moves through the digestive tract. This is largely regulated by the vagus nerve, the key highway of the gut-brain axis. When the vagus nerve is affected by head trauma, gut motility can become erratic, resulting in symptoms such as constipation, reflux, nausea, or bloating (13). In some cases, this can persist for weeks and further reduce appetite or nutrient absorption during a critical healing phase
These factors are important because inflammation that is happening in the gut can reach the brain and potentially worsen post-concussion symptoms like brain fog, mood swings, or fatigue.
The good news, however, is that this two-way street means healing the gut can also support the brain. And through targeted foods and lifestyle habits, you can nourish both ends of the gut-brain connection.
What About The Long Term Effects of Concussion?
If your child isn’t bouncing back as expected, or their symptoms keep flaring up with activity or stress, it’s worth exploring further. That lingering sense that “they’re just not quite themselves” can be very real, and they might be dealing with Post Concussion Syndrome (PCS) - a condition where concussion-related symptoms persist longer than expected. While PCS is more often discussed in adults, research shows that it can and does occur in children and adolescents (14, 15), though it may be under-recognised or misattributed to behavioural or emotional issues.
What Is Post Concussion Syndrome In Children?
Post Concussion Syndrome can show up in different ways for different kids. Some may still have a daily headache; others are just not quite right. Common lingering symptoms can include:
Ongoing headaches or pressure in the head
Fatigue or low energy
Trouble concentrating or memory issues
Irritability, mood swings, or anxiety
Sleep disturbances (difficulty falling asleep, waking up frequently)
Sensitivity to light or sound
Feeling “foggy” or slowed down
Dizziness or balance issues
These symptoms can significantly impact a child’s daily functioning, especially at school, during sports, and in social situations. And because kids may have trouble articulating what they're feeling, these symptoms might show up as irritability, school avoidance, or changes in appetite, behaviour, or energy.
Why Does Post Concussion Syndrome Happen?
Post-concussion syndrome (PCS) can occur when deeper factors are interfering with recovery. In the clinic, we consider factors such as poor inflammatory regulation, nutrient deficiencies, a disrupted gut microbiome, or impaired mitochondrial function. Genetics can also play a role, and for an individual approach we often consider variations to gene SNPs such as SLC17A7 and APOE (16, 17), that can affect how well a child calms inflammation, detoxifies, produces and clears key neurotransmitters.
It's usually not just one factor, but often a combination of drivers that contribute to lingering symptoms and this is where a naturopathic approach can be helpful: it’s about looking at the whole picture, identifying what might be slowing healing and creating a personalised plan that may include nutrition, calming herbs, mitochondrial support, and strategies to restore gut and nervous system balance.
What to Do After a Concussion to Support Long Term Recovery
Once your child has moved through the early stages of concussion recovery, you might be wondering: “Now what?”. The truth is, concussion recovery doesn’t always end when the headaches stop. This next phase is about shifting from rest to active repair - nurturing the brain, restoring energy, and supporting emotional balance. It’s also where ongoing guidance can make a real difference in helping kids regain their confidence, well-being, and resilience.
So, whether you're still navigating how to treat a concussion in a child in that initial recovery stage, or starting to think about how to prevent long term effects of a concussion, there are simple, evidence-informed, parent-friendly steps you can take to help your child’s brain and body heal more fully.
Concussion Recovery Tips for Kids: Healing at Home
The good news is that you can begin supporting brain healing at home with a few smart tweaks to nutrition and routines - things like meals that fuel the brain, consistent sleep, good hydration, and reducing screen time. These small but powerful changes help lower inflammation, stabilise mood, and provide the brain with the building blocks it needs to heal.
Focus on Brain-Loving Nutrition
As nutritionists, we’re big fans of food as medicine! The brain is incredibly nutrient-hungry, especially during recovery from a concussion. It’s working hard to repair damaged neurons, reduce inflammation, and restore normal function. To do that, it needs a steady supply of nutrients that specifically support these processes. The best foods for concussion recovery are anti-inflammatory, antioxidant-rich, and packed with the building blocks for cellular repair and brain function.
Here’s what to prioritise:
Also include plenty of prebiotic fibres from oats, bananas, pears, legumes, and veggies, which feed beneficial bacteria and support production of short-chain fatty acids like butyrate, known to calm gut and brain inflammation (18).
And lastly, don’t forget hydration, as dehydration worsens brain fog and fatigue. Try filtered water, coconut water, or look for natural electrolyte powders with no additives or colours.
Foods to avoid:
Just as important as what to include is what to limit. The worst foods for concussion recovery are those that are ultra-processed, high in sugar, or made with inflammatory oils (like seed oils often found in packaged snacks and fast food). These can interfere with healing, worsen inflammation, and contribute to brain fog and energy crashes.
Prioritise Deep, Restorative Sleep
In case it’s not clear by now just how important sleep and rest are for concussion recovery, I’ll say it one more time - they are essential foundations for overall brain health and effective healing! To support healthy sleep post concussion:
Avoid screens 1–2 hours before bed, as blue light from tablets, phones, and TVs can suppress melatonin production, interfering with the natural sleep–wake rhythm.
Stick to a regular bedtime and wake time to help regulate the circadian clock and improve melatonin secretion, even on weekends.
Try calming, predictable routines, like a warm bath, dim lighting, calming music, or gentle stretches, to signal to the body that it’s time to rest.
Magnesium (especially magnesium glycinate) helps relax the body and mind and can ease muscle tension or restlessness before bed (more on this soon!)
For ongoing sleep challenges, herbs like Valerian, Lavender, and California Poppy may be helpful, but these should always be prescribed by an experienced practitioner to ensure they’re appropriate and safe for your child’s age, situation and medication use.
Best Supplements For Concussion Recovery
While good nutrition and routines lay the foundation, targeted use of key vitamins or herbal medicine can play a powerful role in supporting healing after injury, particularly when there are lingering symptoms or post-concussion syndrome. The following herbs and nutrients are some of our favourites for supporting brain repair and inflammation.
Important note for parents: Always consult a qualified practitioner before starting supplements, especially in children, as dosages need to be adjusted for age, weight, and individual needs.
Fish Oil & Omega-3 Fatty Acids
Omega-3 fatty acids, especially those found in fish oil, are among the most well-researched nutrients for brain health. Known for their powerful anti-inflammatory properties, omega-3s play an important role in reducing neuroinflammation, supporting cognitive function, mood regulation, and overall brain repair.
After a concussion, boosting DHA and EPA intake can support healing at a cellular level and improve recovery. For example, in a 2022 randomised controlled trial in college athletes found that those taking omega-3 supplements recovered significantly faster after a concussion, with symptoms resolving around 5 days earlier compared to the placebo group (19).
For children, omega-3 dosing should always be individualised under the guidance of a healthcare practitioner. However, a general starting point for post-concussion support is often 500–1000 mg combined EPA and DHA daily, ideally in a high-quality, purified fish oil or algae-based supplement.
Magnesium
Magnesium is one of the most important minerals for a child’s brain during concussion recovery. It helps calm the nervous system, reduce inflammation (20, 21), stabilise the blood-brain barrier (22), and support energy production in brain cells. One of its key roles is helping to regulate brain activity. After a concussion, the brain can become overstimulated, with too much glutamate (a stimulating chemical) and not enough GABA (a natural calming chemical). Magnesium helps restore this balance (22), which can ease anxiety, irritability, restlessness, and sleep issues - common symptoms during recovery.
Additionally, research in children found that magnesium supplementation significantly improved post-concussive symptoms like headache, fatigue, and concentration difficulties when compared to placebo (23). For nervous system support, magnesium glycinate is a gentle, calming option. For more targeted brain recovery, magnesium L-threonate may be beneficial as it crosses the blood-brain barrier (24).
Probiotics
After a concussion, the gut can become inflamed, leaky, and low in beneficial short-chain fatty acids (SCFAs) - all of which can slow brain recovery. Probiotics support healing by restoring gut balance, calming inflammation, and improving gut barrier function (25).
Preclinical studies show that strains like Lactobacillus acidophilus and Bifidobacterium species can reduce systemic inflammation, support gut lining repair, and improve neurological outcomes after brain injury (26). However, it is important to note that probiotic benefits are strain-specific - ie, not all probiotics do the same thing, and we need to choose probiotic strains for their targeted effects.
N-Acetylcysteine (NAC)
N-Acetylcysteine (NAC) is a powerful antioxidant key in reducing oxidative stress and inflammation, two major players in concussion. After a head injury, the brain produces a surge of free radicals and inflammatory molecules that can prolong symptoms. NAC works by replenishing glutathione (27), the body’s master antioxidant, helping to protect brain cells and support recovery.
Vitamin D
Vitamin D is well known for supporting bones and immunity, but it also plays an important role in brain health and recovery from injury. Low vitamin D levels have been linked to worse outcomes, such as longer recovery times, persistent headaches, and mood symptoms (28)
Many children, especially those who spend more time indoors, wear sunscreen, or live in less sunny climates, are at risk of low vitamin D. This makes testing and correcting deficiency an important step in concussion care and supplementing when levels are inadequate.
Curcumin
Curcumin, the active compound in turmeric, is a natural but powerful anti-inflammatory and antioxidant, helpful for calming brain inflammation. Research shows that curcumin can help protect brain cells, reduce inflammation and swelling in the brain, and support cognitive function after brain injury (29, 30).
Branched-Chain Amino Acids (Leucine, Isoleucine, Valine)
After a concussion, the brain goes through an energy crash, where it struggles to produce energy properly, and the balance of neurotransmitters that support mood and focus can be thrown off. Research shows that branch chain amino acids (BCAA) - leucine, isoleucine and valine - supplementation post-concussion has improved cognitive performance, working memory, and motor coordination by supporting mitochondrial function and restoring neurotransmitters, which is especially useful for lingering fogginess, poor mood and attention, or energy dips (31, 32)
Herbal Supports
Herbal medicine can gently help children’s nervous systems heal after a concussion. Two important types are nervines and adaptogens.
Nervines are calming herbs that soothe and regulate the nervous system. They can help with anxiety, trouble sleeping, emotional ups and downs, and restlessness. These herbs work by gently balancing brain chemicals to ease overstimulation without making children feel sleepy or dull. Common nervines include Chamomile, Lemon Balm, and Passionflower - all used to help kids feel calmer and sleep better (33, 34, 35).
Adaptogens are herbs that help the body manage stress and build resilience over time. Instead of just calming the nervous system, they help strengthen it, improving energy, mood, and focus. Adaptogens like Ashwagandha, Rhodiola, and Siberian Ginseng are especially helpful when kids feel tired, foggy, or emotionally overwhelmed after the initial rest period following a concussion (36, 37, 38).
Herbal supports should always be used under the guidance of a healthcare practitioner, who can create the best combination based on each child’s unique needs and recovery stage.
The Bigger Picture: Supporting Your Child’s Full Recovery
Concussion recovery is rarely a straight line, especially for children. While rest is essential in the early stages, long-term healing often needs a more holistic approach. If your child still isn’t quite themselves weeks after the injury, it doesn’t mean you’ve missed something; it just means their brain and body may need a little more support.
From reducing inflammation to restoring gut health, calming the nervous system, and supporting mitochondrial function, there’s a lot we can do to help the brain recover gently and thoroughly. Nutrients, herbs, lifestyle adjustments, and integrative care can all play a role in helping your child feel clear, calm, and back to their vibrant self.
Above all, you know your child best. Subtle signs can signal a need for more support, and with the right care team around you, from your GP to your naturopath, physio, or osteopath, concussion recovery can feel more supported and manageable.
Recovery can take time, but taking a whole-person approach can help ensure no piece of the puzzle is overlooked.
Disclaimer: This article is for educational purposes and does not constitute individual health advice. It is important to seek the advice of your primary health practitioner to assess what is right for you and your child. If you have questions of an individual nature, you are welcome to book a free chat here.
More about Kate Shore - Paediatric Naturopath:
Kate is a children’s naturopath with a special interest and clinical focus on mental health and neuropsychiatric conditions in kids. She received her Bachelor of Health Science from Torrens University and has established her practice in North Warrandyte, Melbourne, where she sees clients both in person and via telehealth. Her approach draws heavily on nutrigenomics, microbiome testing, nutritional foundations, and lifestyle support. She works with a range of children and conditions, from anxiety and depression, ADHD and autism, OCD, and PANS/PANDAS.
If you want to get in touch or have any more questions about the above, you are welcome to get in touch here or make an time for a free chat here.
If you want to keep learning, you can read the research here:
Halstead, M. E., Walter, K. D., Moffatt, K., Council on Sports Medicine and Fitness, LaBella, C. R., Brooks, M. A., ... & Stricker, P. R. (2018). Sport-related concussion in children and adolescents. Pediatrics, 142(6), e20183074. https://doi.org/10.1542/peds.2018-3074
McCrory, P., Collie, A., Anderson, V., & Davis, G. (2004). Can we manage sport related concussion in children the same as in adults?. British journal of sports medicine, 38(5), 516-519. https://doi.org/10.1136/bjsm.2004.014811
Manzanero, S., Elkington, L. J., Praet, S. F., Lovell, G., Waddington, G., & Hughes, D. C. (2017). Post-concussion recovery in children and adolescents: A narrative review. Journal of concussion, 1, 2059700217726874. https://doi.org/10.1177/2059700217726874
Cassimatis, M., Orr, R., Fyffe, A., & Browne, G. (2021). Early injury evaluation following concussion is associated with improved recovery time in children and adolescents. Journal of science and medicine in sport, 24(12), 1235-1239. https://doi.org/10.1016/j.jsams.2021.06.012
De Oliveira, N., Horsey, J., Vanleuven, J., Williams, K. L., Zuckerman, S. L., & Terry, D. P. (2025). Does the presence of acute sleep initiation symptoms impact recovery from sport-related concussion?. Brain Injury, 1-10. https://doi.org/10.1080/02699052.2025.2525102
Butterfield, L., Zemek, R., Borghese, M. M., Bijelic, V., Barrowman, N., Sicard, V., ... & Borghese, M. (2025). Nightly Sleep Duration and Symptom Burden Over 1 Month Following Pediatric Concussion. JAMA Network Open, 8(6), e2516333-e2516333. doi:10.1001/jamanetworkopen.2025.16333
Leddy, J. J., Haider, M. N., Ellis, M. J., Mannix, R., Darling, S. R., Freitas, M. S., Suffoletto, H. N., Leiter, J., Cordingley, D. M., & Willer, B. (2019). Early Subthreshold Aerobic Exercise for Sport-Related Concussion: A Randomized Clinical Trial. JAMA pediatrics, 173(4), 319–325. https://doi.org/10.1001/jamapediatrics.2018.4397
van Ierssel, J., Osmond, M., Hamid, J., Sampson, M., & Zemek, R. (2021). What is the risk of recurrent concussion in children and adolescents aged 5–18 years? A systematic review and meta-analysis. British journal of sports medicine, 55(12), 663-669. https://doi.org/10.1136/bjsports-2020-102967
Gornall, A., Takagi, M., Morawakage, T., Liu, X., & Anderson, V. (2021). Mental health after paediatric concussion: a systematic review and meta-analysis. British journal of sports medicine, 55(18), 1048-1058. https://doi.org/10.1136/bjsports-2020-103548
Hanscom, M., Loane, D. J., & Shea-Donohue, T. (2021). Brain-gut axis dysfunction in the pathogenesis of traumatic brain injury. The Journal of Clinical Investigation, 131(12), e143777. https://doi.org/10.1172/JCI143777
Soriano, S., Curry, K., Sadrameli, S. S., Wang, Q., Nute, M., Reeves, E., Kabir, R., Wiese, J., Criswell, A., Schodrof, S., Britz, G. W., Gadhia, R., Podell, K., Treangen, T., & Villapol, S. (2022). Alterations to the gut microbiome after sport-related concussion in a collegiate football players cohort: A pilot study. Brain, Behaviour, & Bmmunity - Health, 21, 100438. https://doi.org/10.1016/j.bbih.2022.100438
Kharrazian D. (2015). Traumatic Brain Injury and the Effect on the Brain-Gut Axis. Alternative therapies in health and medicine, 21 Suppl 3, 28–32. https://pubmed.ncbi.nlm.nih.gov/26348611/
Barlow, K. M., Crawford, S., Stevenson, A., Sandhu, S. S., Belanger, F., & Dewey, D. (2010). Epidemiology of postconcussion syndrome in pediatric mild traumatic brain injury. Pediatrics, 126(2), e374-e381. https://doi.org/10.1542/peds.2009-0925
Fried, E., Balla, U., Catalogna, M., Kozer, E., Oren-Amit, A., Hadanny, A., & Efrati, S. (2022). Persistent post-concussive syndrome in children after mild traumatic brain injury is prevalent and vastly underdiagnosed. Scientific reports, 12(1), 4364. https://doi.org/10.1038/s41598-022-08302-0
Madura, S. A., McDevitt, J. K., Tierney, R. T., Mansell, J. L., Hayes, D. J., Gaughan, J. P., & Krynetskiy, E. (2016). Genetic variation in SLC17A7 promoter associated with response to sport-related concussions. Brain injury, 30(7), 908-913. https://doi.org/10.3109/02699052.2016.1146958
Panenka, W. J., Gardner, A. J., Dretsch, M. N., Crynen, G. C., Crawford, F. C., & Iverson, G. L. (2017). Systematic review of genetic risk factors for sustaining a mild traumatic brain injury. Journal of Neurotrauma, 34(13), 2093-2099. https://doi.org/10.1089/neu.2016.4833
Yanckello, L. M., Fanelli, B., McCulloch, S., Xing, X., Sun, M., Hammond, T. C., Colwell, R., Gu, Z., Ericsson, A. C., Chang, Y. H., Bachstetter, A. D., & Lin, A. L. (2022). Inulin Supplementation Mitigates Gut Dysbiosis and Brain Impairment Induced by Mild Traumatic Brain Injury during Chronic Phase. Journal of cellular immunology, 4(2), 50–64. https://doi.org/10.33696/immunology.4.132
Miller, S. M., Zynda, A. J., Sabatino, M. J., Jo, C., Ellis, H. B., & Dimeff, R. J. (2022). A Pilot Randomized Controlled Trial of Docosahexaenoic Acid for the Treatment of Sport-Related Concussion in Adolescents. Clinical pediatrics, 61(11), 785–794. https://doi.org/10.1177/00099228221101726
Kirkland, A. E., Sarlo, G. L., & Holton, K. F. (2018). The Role of Magnesium in Neurological Disorders. Nutrients, 10(6), 730. https://doi.org/10.3390/nu10060730
Patel, V., Akimbekov, N. S., Grant, W. B., Dean, C., Fang, X., & Razzaque, M. S. (2024). Neuroprotective effects of magnesium: Implications for neuroinflammation and cognitive decline. Frontiers in Endocrinology, 15, 1406455. https://doi.org/10.3389/fendo.2024.1406455
Maier, J. A., Locatelli, L., Fedele, G., Cazzaniga, A., & Mazur, A. (2022). Magnesium and the brain: A focus on neuroinflammation and neurodegeneration. International journal of molecular sciences, 24(1), 223. https://doi.org/10.3390/ijms24010223
Standiford, L., O'Daniel, M., Hysell, M., & Trigger, C. (2021). A randomized cohort study of the efficacy of PO magnesium in the treatment of acute concussions in adolescents. The American journal of emergency medicine, 44, 419–422. https://doi.org/10.1016/j.ajem.2020.05.010
Shen, Y., Dai, L., Tian, H., Xu, R., Li, F., Li, Z., Zhou, J., Wang, L., Dong, J., & Sun, L. (2019). Treatment Of Magnesium-L-Threonate Elevates The Magnesium Level In The Cerebrospinal Fluid And Attenuates Motor Deficits And Dopamine Neuron Loss In A Mouse Model Of Parkinson's disease. Neuropsychiatric disease and treatment, 15, 3143–3153. https://doi.org/10.2147/NDT.S230688
Pagkou, D., Kogias, E., Foroglou, N., & Kotzampassi, K. (2024). Probiotics in Traumatic Brain Injury: New Insights into Mechanisms and Future Perspectives. Journal of Clinical Medicine, 13(15), 4546. https://doi.org/10.3390/jcm13154546
Albert, V., Subramanian, A., & Agrawal, D. (2025). Role of the gut-brain axis in severe traumatic brain injury: insights from experimental models and clinical studies. Indian Journal of Neurotrauma. 10.1055/s-0045-1807265
Samuni, Y., Goldstein, S., Dean, O. M., & Berk, M. (2013). The chemistry and biological activities of N-acetylcysteine. Biochimica et Biophysica Acta (BBA)-General Subjects, 1830(8), 4117-4129. https://doi.org/10.1016/j.bbagen.2013.04.016
Choudhary, A., Kumar, A., Sharma, R., Khurana, L., Jain, S., Sharma, S., … Sharma, S. (2021). Optimal vitamin D level ameliorates neurological outcome and quality of life after traumatic brain injury: a clinical perspective. International Journal of Neuroscience, 133(4), 417–425. https://doi.org/10.1080/00207454.2021.1924706
Wu A, Ying Z, Gomez-Pinilla F. Dietary curcumin counteracts the outcome of traumatic brain injury on oxidative stress, synaptic plasticity, and cognition. Exp Neurol. 2006;197(2):309–317. https://doi.org/10.1016/j.expneurol.2005.09.004
Sharma, S., Kulkarni, S. K., & Chopra, K. (2006). Curcumin, the active principle of turmeric (Curcuma longa), ameliorates diabetic nephropathy in rats. Clinical and experimental pharmacology & physiology, 33(10), 940–945. https://doi.org/10.1111/j.1440-1681.2006.04468.x
Pinheiro, J. L., Rocha, A., & Pinheiro, J. (2018). Traumatic brain injury and branched-chain amino acids. J Clin Nutr Metab 2, 1, 2.
Sharma, B., Lawrence, D. W., & Hutchison, M. G. (2018). Branched Chain Amino Acids (BCAAs) and Traumatic Brain Injury: A Systematic Review. The Journal of head trauma rehabilitation, 33(1), 33–45. https://doi.org/10.1097/HTR.0000000000000280
Kazemi, A., Shojaei-Zarghani, S., Eskandarzadeh, P., & Hashempur, M. H. (2024). Effects of chamomile (Matricaria chamomilla L.) on sleep: A systematic review and meta-analysis of clinical trials. Complementary Therapies in Medicine, 103071. https://doi.org/10.1016/j.ctim.2024.103071
Mathews, I. M., Eastwood, J., Lamport, D. J., Cozannet, R. L., Fanca-Berthon, P., & Williams, C. M. (2024). Clinical Efficacy and Tolerability of Lemon Balm (Melissa officinalis L.) in Psychological Well-Being: A Review. Nutrients, 16(20), 3545. https://doi.org/10.3390/nu16203545
Walsh, K. R. (2025). Examining the Anxiolytic Effects of Flavonoids in Passionflower: A Gut-Brain Axis Perspective. PSU McNair Scholars Online Journal, 17(1), 5. 10.15760/mcnair.2025.17.1.5
Ng, Q. X., Loke, W., Foo, N. X., Tan, W. J., Chan, H. W., Lim, D. Y., & Yeo, W. S. (2020). A systematic review of the clinical use of Withania somnifera (Ashwagandha) to ameliorate cognitive dysfunction. Phytotherapy Research, 34(3), 583-590. https://doi.org/10.1002/ptr.6552
Ivanova Stojcheva, E., & Quintela, J. C. (2022). The Effectiveness of Rhodiola rosea L. Preparations in Alleviating Various Aspects of Life-Stress Symptoms and Stress-Induced Conditions—Encouraging Clinical Evidence. Molecules, 27(12), 3902. https://doi.org/10.3390/molecules27123902
Li, X. T., Zhou, J. C., Zhou, Y., Ren, Y. S., Huang, Y. H., Wang, S. M., ... & Ge, Y. W. (2022). Pharmacological effects of Eleutherococcus senticosus on the neurological disorders. Phytotherapy Research, 36(9), 3490-3504. https://doi.org/10.1002/ptr.7555